Our full-service medical billing covers the entire billing cycle—from patient registration to final payment collection—ensuring accurate, timely reimbursements.
🔹 Claim Submission & Follow-Ups – We submit error-free claims and actively track them to prevent delays.
🔹 Denial Management & Appeals – If a claim is denied, our team swiftly investigates, corrects, and resubmits.
🔹 Accurate Coding & Compliance – We use ICD-10, CPT, and HCPCS coding standards to ensure compliance and minimize errors.
🔹 Payment Posting & Reconciliation – We accurately record payments and reconcile accounts for financial clarity.
✔️ Reduced claim denials
✔️ Faster reimbursements
✔️ Higher revenue collection

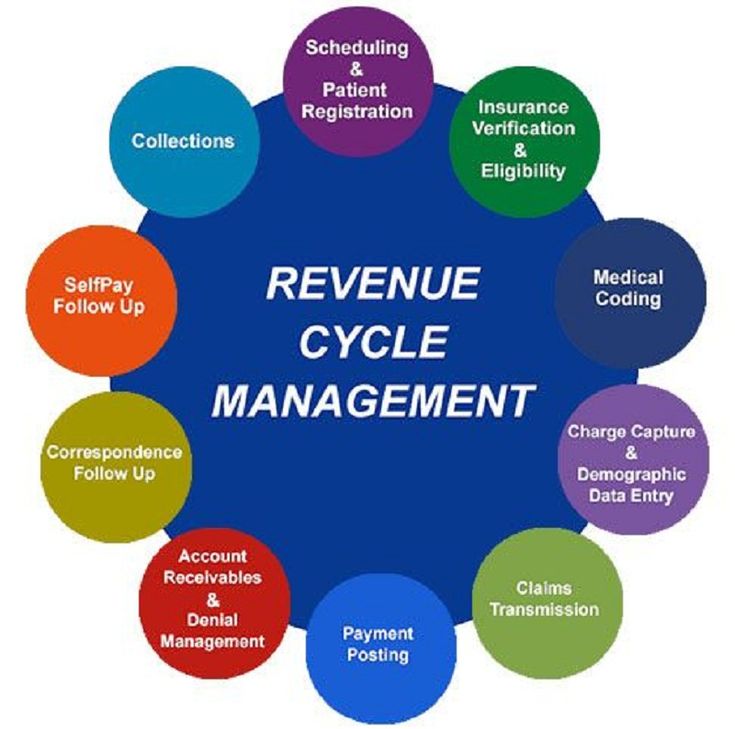
We take a data-driven approach to RCM, ensuring healthcare providers receive the payments they deserve without disruptions.
🔹 Charge Entry & Claim Scrubbing – We meticulously review charges before claim submission to eliminate errors.
🔹 Accounts Receivable (A/R) Management – Our specialists follow up on outstanding payments and ensure prompt collection.
🔹 Financial Reporting & Analytics – Get customized reports that provide insight into your practice’s financial performance.
🔹 HIPAA-Compliant Workflows – Ensuring all processes adhere to industry regulations to protect patient data.
✔️ Increase collections by up to 30%
✔️ Lower A/R days
✔️ Improve financial transparency
Our team of AAPC-certified coders ensures precise ICD-10, CPT, and HCPCS coding, minimizing claim rejections and improving revenue recovery rates.
🔹 Specialty-Specific Coding – Expertise in Cardiology, Radiology, Orthopedics, Internal Medicine, and more.
🔹 Regular Audits – We conduct internal audits to ensure coding accuracy and compliance.
🔹 Claim Reconciliation – Fixing underpayments and resolving coding-related denials.
✔️ Up to 98% claim acceptance rate
✔️ Avoid compliance risks & audits
✔️ Maximize insurance reimbursements

We handle the complex credentialing process, ensuring providers are enrolled with the right insurance networks for faster payments.
🔹 New Provider Enrollment – We manage all documentation and payer applications.
🔹 Re-Credentialing & Maintenance – Keeping credentials up to date to avoid billing interruptions.
🔹 CAQH Profile Management – Ensuring provider information is verified and current with insurance payers.
🔹 Contract Negotiations – Securing the best reimbursement rates for your practice.
✔️ Speed up payer approvals
✔️ Reduce claim denials due to credentialing issues
✔️ Ensure uninterrupted insurance payments
We check patient insurance eligibility in real-time, ensuring correct coverage details before service is provided.
🔹 Eligibility & Benefits Verification – Checking copays, deductibles, and policy status.
🔹 Prior Authorization Handling – Faster approvals for procedures requiring insurance authorization.
🔹 Real-Time Verification – Reducing billing errors and patient payment confusion.
✔️Reduce claim rejections by 40%
✔️ Improve cash flow with pre-verified coverage
✔️ Enhance patient satisfaction with upfront transparency


We aggressively track, analyze, and appeal denied claims to maximize revenue recovery.
🔹 Root Cause Analysis – Identifying denial trends and fixing underlying billing issues.
🔹 Appeals & Resubmissions – Expert handling of insurance appeals for quick resolution.
🔹 Preventative Solutions – Implementing strategies to avoid future denials.
✔️ Reduce denials by up to 80%
✔️ Faster claim approvals
✔️ Increased revenue retention
We provide easy-to-understand billing statements and online payment options, improving collections and patient satisfaction.
🔹 Custom Patient Statements – Sending clear, detailed invoices to avoid confusion.
🔹 Payment Plans & Online Portals – Offering flexible payment options to increase patient collections.
🔹 Billing Support & Dispute Resolution – Handling patient inquiries professionally.
✔️ Reduce unpaid patient balances
✔️Improve patient trust with clear billing
✔️ Enhance collections with digital payment options


We ensure your billing operations comply with CMS, HIPAA, and payer-specific regulations.
🔹 Regular Internal Audits – Checking for billing inefficiencies, coding errors, and fraud risks.
🔹 HIPAA Compliance Assurance – Ensuring patient data security and regulatory adherence.
🔹 Risk Assessment & Corrective Action – Identifying issues before they become legal or financial risks.
✔️ Stay compliant & avoid penalties
✔️Identify and fix revenue leaks
✔️Maintain a clean audit record
We provide detailed analytics and performance reports to help you make data-driven decisions.
🔹 Revenue & Cash Flow Analysis – Understanding your practice’s financial health.
🔹 Claim Performance Tracking – Identifying areas of improvement for faster reimbursements.
🔹 Custom Reports & Dashboards – Get reports tailored to your business needs.
✔️ Improve practice efficiency
✔️ Maximize profitability
✔️ Reduce financial bottlenecks

Your Trusted Partner for Seamless Medical Billing & Revenue Optimization
Minimize errors & maximize reimbursements
Secure and regulation-friendly billing practices
A dedicated team of certified professionals
Accelerate reimbursements with real-time claim tracking.
ailored to meet your practice’s unique needs
Reliable and responsive customer service